Childhood asthma isn't a different disease from asthma in adults, but children face unique challenges that can interfere with their development in daily activities such as playing sports, going to school and sleeping.
Although it's a chronic condition, the right and continuous treatment is the key to keep asthma under control so children can feel better and live a healthy and active life. Take the control in childhood asthma. Ask your doctor for advice.
Childhood Asthma
Did you know that asthma is the most common chronic pulmonary condition in children?1 Poorly managed and undiagnosed asthma in young children can lead to visits to the emergency room, hospital stays, missed workdays for parents and suffering that many young children can't express.2
What is Asthma?
Asthma Sympthoms
Diagnosis
Treatment
Myths vs Facts
Asthma is one of the most common chronic childhood conditions1, but there are still many myths and misunderstandings about it. Read on for the most common myths and why they need busting.
Daily Care
Asthma is a chronic inflamatory disease that is episodic, meaning that symptoms can come and go. The good news is that you can find support to help you manage your child’s asthma and create asthma-friendly environments so he/she can live an active and healthy life.

Tips for kids
Managing asthma in children under 5 years old can be difficult. Sometimes your child may be frustrated, angry or sad because they need to cut their usual activities to avoid the triggers. Treatment with nebulizers can also bring difficulties, babies and young children may be frightened by the appearance and noise of the device, but there are tricks that can make the whole process more pleasant for them. Here are some tips that can help you keep asthma under control so your children can feel better and live a more healthy and active life.
How can I treat my child’s asthma at home?

- Making nebulization a special experience:
- Make the mask special by decorating it with cheerful makeup or stickers, and give the nebulizer a fun name.14,17
- Role Play: pretend with your child that he or she is a firefighter, astronaut, pilot, or alien once the mask goes on and play along during treatment.17
- Make your child more involved in the treatment process:
- If possible, involve them in the choosing process. There are several kid-friendly models of nebulizers.17
- Let your child be “in charge” of nebulizing by putting on the mask or turning the machine on and off.17
- Make treatment part of the routine:
- Use the nebulizer at the same time each day so that your child knows what to expect.14,17
- Try nebulizing as part of the morning routine between eating breakfast and brushing your child’s teeth.17
What recommendations should I follow when a child with asthma exercises or plays?

- Monitor your child during activity and have rescue medication handy.9
- Make sure your child knows the signs of an asthma attack and how to respond.9,16
- If your child is in daycare or school or day care, make sure the nurse, teachers and coaches know about your child’s asthma, can recognize signs of an asthma attack, and can respond when needed.16
- Make sure your child has a good warm up period of about 5 to 10 minutes of stretching and light activity before starting any vigorous activity. Cooling down is just as important and so is keeping your child well hydrated.9,16
Taking these steps will help your child to breathe easier and reduce the chances of having severe symptoms and asthma attacks.
What can I do to help my child sleep better?

- Keep a clean bedroom environment.4,18
- Make sure to change sheets regularly, wash bedding in hot water, and wipe down shelves, ledges or nearby furniture to minimize dust. Don’t let your child sleep in the same room with pets.4,18
- Choose allergy-free linens. Make sure pillows have a cover and look for allergy-free materials.18
- Use a humidifier. Keep the air moist in your child’s room with a humidifier.18
If your child suffers from asthma symptoms at night regularly, call your child’s doctor.
What to pack when travelling

- Medicines: Keep quick-relief medicine (also called rescue or fast-acting medicine) and long-term control medicine (also called controller, preventer or maintenance medicine) handy, not buried in the car trunk. If you're flying, take them in your carry-on luggage. That way, you'll have them if needed during the flight or if your checked bags go astray. Time zone changes can be tricky. While traveling, try to have your child take medicines at the usual home time. Upon arrival in another time zone, adjust the dosage times to the local clock.19
- Nebulizer: If your child uses one, you might want to get a portable version. Many of these can be plugged into a car's accessory power outlet (or the cigarette lighter in older vehicles). If you're traveling abroad, make sure you have the adapter you need to use it.19
- Peak flow meter: if your child uses one.
How can I use a nebulizer?

Before using a nebulizer with your child, remember to read all the instructions. You can supplement the instructions with the Nebulization Guide for Parents that we have prepared and the video on how to use a compressor nebulizer.
If you have any questions about how to use a nebulizer, contact your child's doctor or the manufacturer.

Is your child's asthma under control?
Fill the respiratory control assessment to find out. 20
ATTENTION: the above questionnaire is not a substitute for the diagnosis or assessment by the treating physician, it is only intended to promote discussion with the healthcare professional about the findings on the control of the disease, so it is important to visit the doctor. Discuss the results with your doctor, especially if the result is "Not well" controlled” or “Very poorly controlled”.
This content is not medical advice or a clinical diagnostic. This is preventive information designed for you to share it with your doctor to inform him about your asthma management. DO NOT STOP OR CHANGE your asthma medication without consulting your health care professional. Always ask your doctor before making any decisions related to your disease.
CC-6058 Set 2023
FAQ
-
What is asthma?
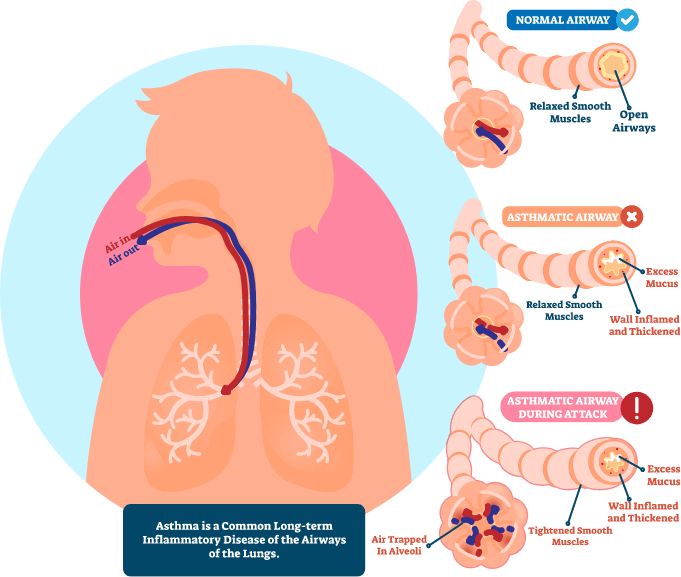
Asthma is a common chronic disease associated to inflammation of the airways, which become narrower and extra-sensitive to irritants. Asthma symptoms include cough, wheezing, shortness of breath, and chest tightness, and may vary over time in frequency and intensity.
-
What causes asthma?
The causes of asthma are not fully understood. Asthma is probably usually caused by a mixture of hereditary factors and environmental factors, but how these factors work together is still largely unknown. Allergens from house dust mites and pets are the most common causes, but many other allergens, such as pollen and moulds, can cause asthma. However, some patients with asthma have no confirmed allergies. 2
-
What are the risk factors for asthma?
Asthma tends to run in families, which means that a child is more likely to develop asthma if someone in the family has it.3 Children with eczema or food allergies are more likely to develop asthma compared to others. Allergies to pollen, house dust mites, or pets also increase the likelihood of developing exacerbations of asthma.3 Exposure to tobacco smoke, air pollution, or other irritants can also cause symptoms in those with an underlying tendency to asthma. Risk factors for childhood asthma are:3
- Allergies or eczema
- Family history of asthma
- Low birth weight
- Exposure to second-hand smoke before or after birth
- Frequent respiratory infections
- Gastroesophageal Reflux Disease (GERD)
-
Will my child outgrow his/her asthma?
Most children who experience breathing difficulties at a young age will never completely grow out of it, but more than 50 percent of children will see a decrease of asthma and allergy symptoms as they grow older. For children who have asthma attacks due to allergens, allergy shots or allergy medications may help reduce the number of acute breathing attacks.4
-
What conditions are associated with asthma?
Children who have allergies to elements of the environment such as pollen, animals, mould, dust and food are more likely to have asthma. Asthma is more likely to develop in children who were born prematurely. 5
-
Are asthma medications dangerous or addictive?
No. Asthma medications are not addictive, and your child will not become “immune” to the beneficial effects by using them regularly. Asthma is different in every patient, and symptoms can change over time. The doctor will determine which asthma medication is best. At recommended doses, asthma medications are safe when used properly.5
-
At what age does asthma start?
Asthma can start at any age, although about half of all people with asthma have had their first symptoms by the age of 10, and many children with asthma have had their first asthma attack before the age of 6.4
-
Can we have pets even though my child has asthma?
If your kid has asthma and is allergic, you should not have a pet. If your child has asthma but no signs of allergy, plus not obvious symptoms from pets, it is probably all right to keep a pet in the family, but bear in mind that it will contribute to the amount of dust in the house. 6
-
How do I know if my child’s asthma is controlled?
Well controlled asthma in children means all the following:2,5,6
- Decreased or no asthma symptoms (cough, wheezing or shortness of breath) on a day to day basis
- No acute asthma episodes or attacks (including ER visits or hospitalizations)
- Not requiring oral steroids (prednisone) more than once per year
- No limitations on activities or school attendance
- No more than twice a week use of quick acting rescue medicines.
-
What are asthma triggers?
Asthma triggers are factors that can cause or worsen asthma symptoms, and even lead to an asthma attack by increasing the inflammation in the airways. The following triggers can cause asthma symptoms and/or start an asthma attack:2,6
- infections, usually those caused by a virus (e.g. colds or flu)
- exercise, especially in cold weather
- emotions, such as excitement, fear or anger
- chest pressure
- laughing
- food additives, such as tartrazine (an artificial food colouring), or food allergens, such as peanuts (sensitised or allergic individuals can have a very severe allergic reaction)
- certain medications -some children may be allergic to some drugs (e.g. aspirin)
- allergens: Once your child is sensitised or allergic, both indoor and outdoor allergens, even small amounts, can cause asthma symptoms and attacks, as well as other allergic symptoms such as sneezing or a runny nose.2,3 It is therefore important to know whether your child’s asthma is caused or worsened by allergens.
Also, many irritating particles or chemicals in the air can trigger an asthma attack. Examples include tobacco smoke, diesel exhaust, air pollution, perfume or other strong scents, household sprays, sulphur dioxide, grain or flour dust and sawdust.7
Sudden weather changes (e.g. cold winds, humidity and storms) can too trigger asthma in some children. Some of these sudden changes can cause the release of allergens, such as pollen, that can make asthma worse in children whose asthma is allergy related. Cold air can also have a direct irritant effect on inflamed airways.2,3
-
Should my child take his asthma medications even though he/she is feeling better?
Yes. Remember asthma is a chronic inflammatory disease of the airways, therefore, no inflammation goes away just because the symptoms went away. Some medications, called controllers, need to be taken daily to control the inflammation present in the lungs of asthmatic people.1,2,5 If your child needs daily controller asthma medication, but does not always take it, asthma symptoms can worsen and may cause a serious asthma attack. That’s why you should always keep track and take care of your child’s treatment. 5
-
Does inhaled corticosteroids stunts growth in children?
Many parents are concerned about the side effects that a daily controller treatment with inhaled corticosteroids may have.
Recent studies found that children with asthma who had received long-term treatment with inhaled corticosteroid attained normal adult height.9 Furthermore, we found no evidence of a dose–response relation between the mean daily dose of inhaled corticosteroid, the cumulative dose of inhaled corticosteroid, or the duration of inhaled steroid treatment and the difference between the measured and target adult heights.8
Apart from the (fortunately low) risk of dying from asthma, there is also a risk that lung function will deteriorate over the years. These risks make it important to assess whether your child’s asthma is really under control and to learn what treatment your child might need to help prevent permanent lung damage. 9
-
What are the most common symptoms of childhood asthma?
Asthma symptoms typically come and go. Most common symptoms include trouble in breathing, chest tightness, wheezing or cough.2,4 These symptoms normally occur during physical activity and at night/sleep. Other common symptoms of childhood asthma are:4
- Intermittent or frequent coughing spells
- Chronic cough
- Wheezing or whistling upon exhale
- Shortness of breath
- Chest tightness or pain
- Weakness or tiredness
- Delayed recovery after a respiratory infection
-
What is an asthma attack?
An asthma attack is a sudden worsening of asthma symptoms. In asthmatic children, the airways are inflamed. During an asthma attack, this inflammation gets worse, the muscles around the airways contract, and excessive mucus is produced, limiting the air that flows in and out of the lungs.2,3,6,11 When asthma is under good control, the airways are clear and air flows easily in and out.
Other indications that your child is suffering from an asthma attack:3- Cannot complete a sentence without catching their breath
- Widens the nostrils to get air
- Use the abdominal or stomach muscles to breathe and is struggling to take a deep breath
-
What happens during an asthma attack?
When asthma is not under control, the airways become inflamed. Inflammation of the airways causes asthma symptoms (wheezing, breathlessness, chest tightness and coughing) by restricting or limiting the airflow to and from the lungs.10
- The airways become red and swollen, which makes them narrower. This can often take several hours or days to develop and may take just as long to reverse after the asthma attack has passed.6,10
- Tightening of the muscles that surround the airways (also called bronchoconstriction) makes them even narrower. This tightening can happen very quickly, depending on the type of trigger and underlying flammation.6,10
- The airways make more mucus, which can plug up or partly block the airways.6,10
The severity of the attacks can range from mild to severe.6,11
-
What should I do when my child has an asthma attack?
If your child has an acute asthma attack, there are several steps you can take to ensure their health and safety. First, remain calm. Staying calm and level-headed will allow you to make the best decisions for your child. Second, have them use their medication according to the doctor’s instructions and help them calm down as much as possible, keeping calm can help keep their airway open. If your child cannot calm his or her breathing even after using medication, you should immediately call your local emergency number or go to the hospital.4
-
What are the signs of a severe and dangerous asthma attack?
- Symptoms that are rapidly becoming more severe and do not get better even with the reliever medication.3,10
- Symptoms that do not improve at all, or rapidly return after using the reliever medication.3,10
- Difficulty talking because of shortness of breath.3,10
-
How can I best manage my child’s asthma?
The best way to manage your child’s asthma is to treat it preventatively with a controller medication.1,2,6 Regular check-ups with your child’s doctor will help stay on top of breathing problems.
Knowing and avoiding your child’s asthma triggers, maintaining a healthy diet and exercise routine for your child, and reducing allergens or pollutants in your child’s environment will also help you managing your child’s asthma.3,6,7
It is important to ensure your child maintains the doctor’s recommended medication regimen.4 -
What are relievers or airway opener medications?
Relievers or airway openers are medicines that provide rapid relief from appearance or worsening of symptoms of asthma by quickly opening the narrowed airways (dilating the bronchi).6,11 This makes it easier to get air in and out of the lungs. Most airway openers work quickly and can be used to treat an asthma attack.6,11 They can also be called rescue bronchodilators. For children, most common airway openers are short-acting bronchodilators. The most widely used short- and quick-acting airway openers are salbutamol (also known as albuterol) and terbutaline.
-
What are controller medications?
People with asthma present chronic inflammation in the airways. Controllers are medicines that treat this chronic inflammation and prevent asthma attacks.12,13 The most common controller medicines are inhaled corticosteroids, leukotriene receptor antagonists, and oral corticosteroids (prescribed only for severe asthma), which reduce airway inflammation.2,11,13 if used regularly as instructed by the doctor, controller medications help to prevent periods of greater severity of asthma. They may relieve your child of symptoms completely for most of the time as well. If the doctor prescribes an inhaled glucocorticosteroid as treatment, your child must use it regularly, even if there is no wheezing or any other symptoms.2,3,6 Especially because with an uncontrolled inflammation, the airways become swollen, narrower and extra-sensitive. It is good to keep in mind that some degree of inflammation is usually present in the lungs, even when your child is unaware of symptoms, and if asthma is not well controlled, a worsening of the inflammation may occur and lead to an asthma attack.3,6
-
What are glucocorticosteroids or corticosteroids?
Glucocorticosteroids, which are also known as corticosteroids, are anti-inflammatory medicines. They are the most common controller medications used to treat chronic inflammation of the airways and help to prevent asthma attacks. Inhaled glucocorticosteroids are the first treatment option for children under five years old with asthma, due to its high anti-inflammatory effect which ensures reliable asthma symptoms control and lowers the risk of asthma attacks and hospitalizations. The most effective and commonly used are budesonide, beclomethasone and fluticasone. 13
-
Why are glucocorticosteroid medications inhaled?
In asthma, glucocorticosteroids are usually inhaled so that the medicine goes straight to the lining of the airways affected by inflammation. This also greatly reduces the risk of any possible harmful effects on the rest of the body.2,13
The small amount of medicine that goes into the bloodstream is rapidly removed from the body.2,13 -
What effects do these anti-inflammatory medications have?
Asthma is caused by chronic inflammation of the airways, which makes them become swollen, narrower and extra-sensitive to irritants. 1,2,6 Controller medications contain anti-inflammatory medicines, and used regularly as instructed by the doctor, besides treating current inflammation, they prevent further swelling, reduce the narrowing due to muscle tightening, make airways less sensitive to asthma triggers.2,12,13 Anti-inflammatory controller medications are very effective and can control asthma in most children. The most effective anti-inflammatory medicines are the inhaled glucocorticosteroids.14
-
What is the difference between an inhaled corticosteroid and an oral corticosteroid?
Though inhaled and oral corticosteroids work in more or less the same way, they differ in how they are used in the treatment of asthma:15
Inhaled corticosteroids: Because they are delivered directly to the lungs, inhaled steroids require smaller doses (measured in micrograms, mcg), have fewer side effects, and are safer for long-term use. They are considered the first-line controller medication for people with asthma.15
Oral corticosteroids: Because they are delivered systemically (via the bloodstream), oral steroids require larger doses (measured in milligrams, mg), have more side effects, and pose greater harms with long-term use. They are reserved for use in more severe cases. 15
-
Is nebulization safe with COVID-19?
According to medical experts, it is important for patients to continue taking their prescribed asthma medications as usual during the COVID-19 (‘coronavirus disease 2019’) pandemic.16 This includes Inhaled Corticosteroids (ICS) -containing medications. Stopping ICS often leads to potentially dangerous worsening of asthma. As such, your child’s physician may recommend nebulizing outside or in an area where air is not recirculated into the home and surfaces are easily cleaned.17
-
Why should I choose a nebulizer instead of other techniques/devices to treat my child’s asthma?
Inhaled therapy is considered the essential component to treating asthma. The ability to deliver drugs directly to airways as a major advantage of inhaled treatment. That’s because when medications are taken orally, it will take time to pass through the gastrointestinal tract to the bloodstream before the body uses the active substances where they are needed, while a nebulizer delivers medications very quickly and directly to the respiratory tract.7 That is to say nebulizer helps deliver the medication to the necessary target organ; your child’s lungs. Other benefits of using nebulization are:
- Fewer Side Effects
The dosage of medicine needed in nebulizer therapy is lesser as compared to medicines given orally. Thus, nebulizer therapy reduces the risk of side effects compared to oral administration of the same medications.18-20 - Easy to Use
Nebulizers require very little effort to use and it is a preferred device for children. Unlike inhalers, which generally require certain breathing/hand coordination, your child only need to breathe normally during nebulizer therapy. This makes it easier also for a caretaker to administer the medication when the patient is unable to do it themselves. Even babies or severely debilitated people can receive medication by nebulizer.18-20 - Better compliance
The ease of use of nebulizer will motivate asthmatic kids to comply with their recommended daily administration of drugs. Convenience and ease of use affect patient satisfaction. Patient satisfaction correlated with compliance and better outcomes.18-20 - Prevention
Nebulizer treatments can prevent asthma episodes. Inhaled steroids are the most important controller treatment to reduce chronic inflammation present on the airways of young children with asthma and prevent asthma attacks. It also works by reducing swelling and mucus production in the airways. Consequently, the airways will become less sensitive and less likely to be exacerbated by triggers.18-20
- Fewer Side Effects
-
How should I clean my child’s nebulizer?
Cleaning your child nebulizer is recommended after each use to ensure safe and effective medication delivery. Always follow the cleaning instructions provided with the nebulizer and consult the doctor regarding the best cleansing agent for it.7
- Physiopedia. 2020. Asthma. [online] Available at: https://www.physio-pedia.com/Asthma [Accessed 15 October 2020].
- Global Initiative for Asthma, GINA. 2020. Preguntas frecuentes [online]. Available at: https://ginasthma.org/about-us/faqs/ [Accessed 15 Oct 2020].
- WebMD. 2020. Childhood Asthma. [online] Available at: https://www.webmd.com/asthma/children-asthma [Accessed 15 October 2020]
- AGC Pediatrics LLC. 2020. Childhood Asthma Faqs - Calhoun Pediatrician - AGC Pediatrics. [online] Available at: https://www.agcpediatrics.com/childhood-asthma-faqs.html [Accessed 15 October 2020].
- Asthma Center. Frequently Asked Questions [online] Available at: https://www.cincinnatichildrens.org/service/a/asthma/faq. [Accessed 3 November 2020].
- Global Initiative for Asthma, GINA. 2020. Guía para pacientes de GINA. [online] Available at: https://ginasthma.org/wp-content/uploads/2020/02/GINA-Patient-Guide-SPANISH-copy.pdf [Accessed 15 Oct 2020].
- National Asthma Education and Prevention Program . (2014). National Heart, Lung, and Blood Institute. Retrieved from NAEPP: https://www.nhlbi.nih.gov/files/docs/public/lung/asthma_tipsheets.pdf
- Agertoft L, et al. Effect of Long-Term Treatment with Inhaled Budesonide on Adult Height in Children with Asthma. N Engl J Med 2000; 343:1064-1069. Doi: 10.1056/NEJM200010123431502
- Pedersen S. Do inhaled corticosteroids inhibit growth in children?. Am J Respir Crit Care Med. 2001;164(4):521-535. doi:10.1164/ajrccm.164.4.2101050
- Learn how to take control of asthma. Centers for Disease Control and Prevention. https://www.cdc.gov/asthma/faqs.html. Published 2020. Accessed November 3, 2020.
- Chop.edu. 2020. Asthma | Children’s Hospital Of Philadelphia. [online] Available at: https://www.chop.edu/conditions-diseases/asthma [Accessed 15 October 2020]
- Everettclinic.com. 2020. Pediatric Asthma | The Everett Clinic. [online] Available at: https://www.everettclinic.com/health-wellness-library/pediatric-asthma.html [Accessed 15 October 2020]
- Mayo Clinic. 2020. Treating Asthma In Children Ages 5 To 11. [online] Available at: https://www.www.mayoclinic.org/diseases-conditions/childhood-asthma/in-depth/asthma-in-children/art-20044383[Accessed 15 October 2020].
- Cannizzaro, T., 2020. Misconceptions Surrounding Inhaled Corticosteroid Medication. [online] asthma.net/. Available at: https://asthma.net/living/misconceptions-surrounding-inhaled-corticosteroid-medication/ [Accessed 15 October 2020].
- Bass, P. 2020. Verywell Health | What Are the Differences Between Inhaled and Oral Corticosteroids? [online] Available at: https://www.verywellhealth.com/the-difference-between-inhaled-oral-corticosteroids-200612#. [Accessed 15 October 2020]
- Global Initiative for Asthma. 2020. COVID-19 GINA Answers to Frequently Asked Questions on asthma management [online] Available at: https://ginasthma.org/covid-19-gina-answers-to-frequently-asked-questions-on-asthma-management/. [Accessed 3 November 2020]
- Kids Health. 2020. Coronavirus (COVID-19): Caring for Your Child With Asthma. [online] Available at: https://kidshealth.org/en/parents/coronavirus-asthma.html [Accessed 1 June 2021]
- Laube BL, et al. What a pulmonologist should know about the new inhalation therapies. Eur Respir J. 2011. 37(6):1308-31.
- Welch MJ. Nebulization therapy for asthma: a practical guide for the busy pediatrician. Clin Pediatr (Phila). 2008;47(8):744-5
- Welch MJ et al. Evaluation of inhaler device technique in caregivers of young children with asthma. Ped Allergy Immun Pulmo. 2010;23(2):113-20
- WHO. 2017. 10 datos sobre el asma [online] Available at: https://www.who.int/features/factfiles/asthma/es/ [Accessed 15 May 2021].
- Global Initiative for Asthma, GINA. 2020. Preguntas frecuentes [online]. Available at: https://ginasthma.org/about-us/faqs/ [Accessed 15 Oct 2020].
- WHO. 2020. Asthma. [online] Available at: https://www.who.int/news-room/fact-sheets/detail/asthma [Accessed 15 Oct 2020].
- Global Initiative for Asthma, GINA. 2020. Guía para pacientes de GINA. [online] Available at: https://ginasthma.org/wp-content/uploads/2020/02/GINA-Patient-Guide-SPANISH-copy.pdf [Accessed 15 Oct 2020].
- WebMD. 2020. Childhood Asthma. [online] Available at: https://www.webmd.com/asthma/children-asthma [Accessed 15 October 2020]
- Everettclinic.com. 2020. Pediatric Asthma | The Everett Clinic. [online] Available at: https://www.everettclinic.com/health-wellness-library/pediatric-asthma.html [Accessed 15 October 2020]
- Chop.edu. 2020. Asthma | Children’s Hospital Of Philadelphia. [online] Available at: https://www.chop.edu/conditions-diseases/asthma [Accessed 15 October 2020]
- Mayo Clinic. 2020. Treating Asthma In Children Ages 5 To 11. [online] Available at: https://www.www.mayoclinic.org/diseases-conditions/childhood-asthma/in-depth/asthma-in-children/art-20044383[Accessed 15 October 2020].
- Asthma UK. 2020. Help Your Child Stay Active | Asthma UK. [online] Available at: https://www.asthma.org.uk/advice/child/life/exercise/ [Accessed 15 October 2020]
- London Doctors Clinic. 2017. Nine Sports Stars That Suffer From Asthma. [online] Available at: https://www.londondoctorsclinic.co.uk/blog/nine-sports-stars-that-suffer-from-asthma/#:~:text=In%20fact%2C%20it%20has%20recently,10%25%20within%20the%20general%20population. [Accessed 15 October 2020]
- Bass, P. 2020. Verywell Health | What Are the Differences Between Inhaled and Oral Corticosteroids? [online] Available at: https://www.verywellhealth.com/the-difference-between-inhaled-oral-corticosteroids-200612#. [Accessed 15 October 2020]
- Pedersen S. Do inhaled corticosteroids inhibit growth in children?. Am J Respir Crit Care Med. 2001;164(4):521-535. doi:10.1164/ajrccm.164.4.2101050
- McGeachie MJ, Yates KP, Zhou X, et al. Patterns of Growth and Decline in Lung Function in Persistent Childhood Asthma. N Engl J Med. 2016;374(19):1842-1852. doi:10.1056/NEJMoa1513737
- Healthline. 2020. Nebulizers For Babies: How They Work. [online] Available at: https://www.healthline.com/health/nebulizer-for-baby [Accessed 15 October 2020].
- Medicalnewstoday.com. 2020. Intrinsic And Extrinsic Asthma: Causes, Symptoms, And Treatment. [online] Available at: https://www.medicalnewstoday.com/articles/325536 [Accessed 15 October 2020].
- WebMD. 2020. Help Your Child Manage Asthma at School. [online] Available at: https://www.webmd.com/asthma/guide/managing-childs-asthma-school https://www.verywellhealth.com/the-difference-between-inhaled-oral-corticosteroids-200612#.
- Kids Health. 2018. How Can I Help My Child Cooperate While Using the Nebulizer? [online] Available at: https://kidshealth.org/en/parents/cooperate-nebulizer.html [Accessed 15 October 2020].
- National Asthma Education and Prevention Program . 2014. National Heart, Lung, and Blood Institute. [online] Available at: https://www.nhlbi.nih.gov/files/docs/public/lung/asthma_tipsheets.pdf [Accessed 15 October 2020].
- Kids Health. 2017. Travelling and Asthma. [online] Available at: https://kidshealth.org/en/parents/travel-asthma.html [online] Available at:
- Murphy K, et al. Test for Respiratory and Asthma Control in Kids (TRACK): A caregiver-completed questionnaire for preschool-aged children. J Allergy Clin Immunol. 2009; 23(4):834-839